Living with Metastatic Breast Cancer
Article: https://www.lbbc.org/your-journey/living-with-metastatic-breast-cancer
Information and support to move forward
A metastatic breast cancer diagnosis can feel like a shock to the system. If you’ve recently been diagnosed, we know that you may be experiencing intense emotions and uncertainty. At the same time, we also know people are living longer with metastatic breast cancer. Advances in imaging and treatment approaches have helped make that happen.
Adjusting to a diagnosis of metastatic breast cancer is different for each person, and it’s an ongoing process. There may be times when you fear for the future, or you feel less confidence in your body or in the people who support you. These are normal responses to grieving the small, and large, losses metastatic breast cancer can cause. Let yourself experience these emotions. You are not alone. Ask for help when you need it. Many people gain great strength from talking with others who’ve been diagnosed and can share in your experience. Some people find themselves thriving after a metastatic breast cancer diagnosis because of a newfound focus on the parts of life that bring the most meaning.
Video: Newly diagnosed: A guide for understanding a diagnosis of MBC
Whether this is your first breast cancer diagnosis, or you have had breast cancer before, learning you have metastatic breast cancer is likely to be overwhelming. This session with Zanetta Lamar, MD is designed to provide you with the medical information and practical support necessary to help you make informed decisions about your treatment and to get your bearings during the first months after a metastatic diagnosis. This session may also be helpful to those who aren’t newly diagnosed but need a basic understanding of metastatic breast cancer and how it is treated.
Quick facts
- An estimated 169,347 people are living with metastatic breast cancer in the U.S. (JCNI, 2022)
- About 6% of breast cancers are stage IV at first diagnosis. (SEER, 2024)
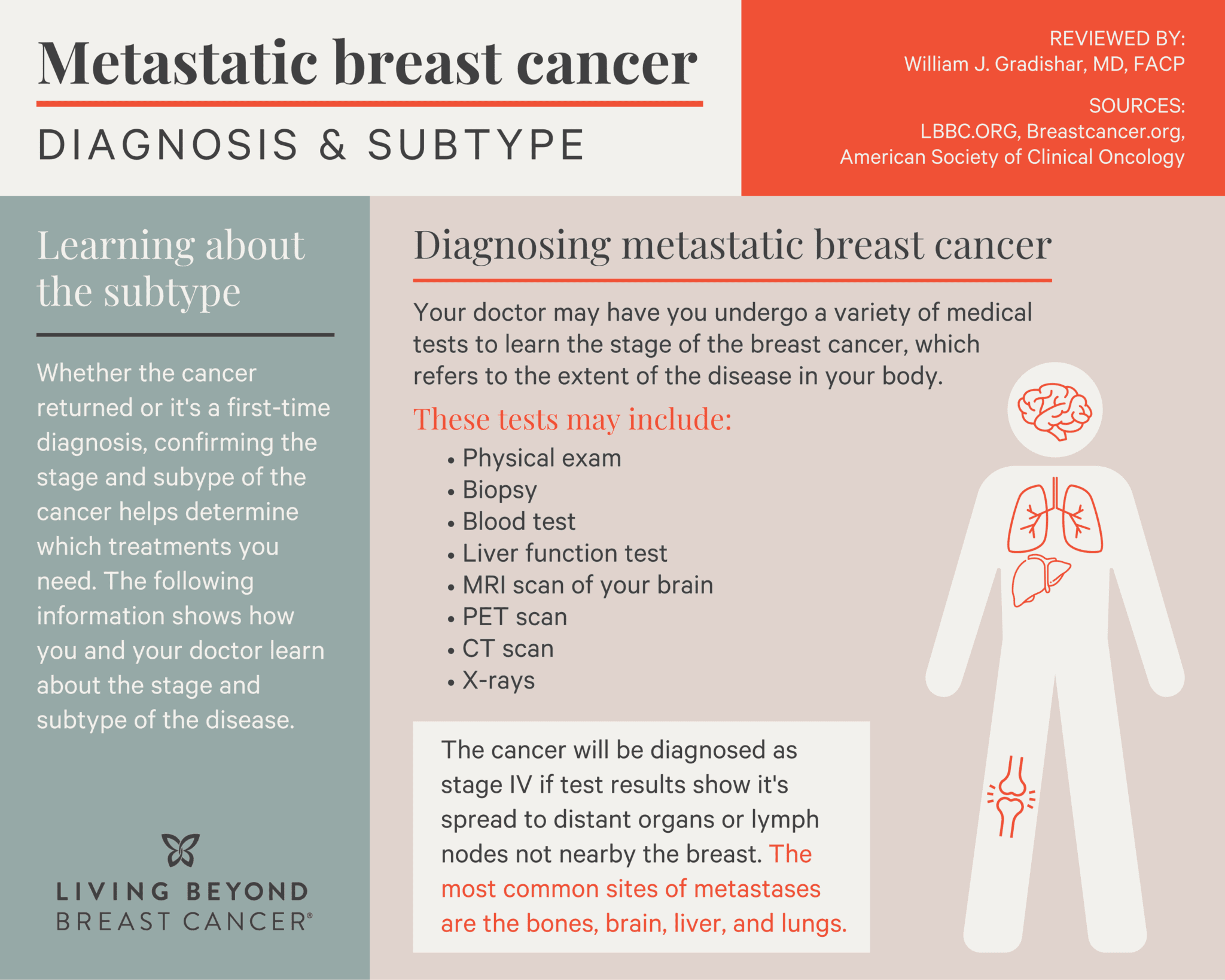
- When breast cancer is stage IV, the most common sites for metastases are the bone, lungs, and liver. (ACS, 2025)
- The goal of MBC treatment is to slow the cancer’s growth, provide relief from its symptoms, and extend life. (ACS, 2025)
Better understand your condition
Understanding more about your situation and treatment options can reduce some of the pressure that comes with the overwhelm of diagnosis. Talking with your doctor, asking questions, and reading trusted resources can often bring a new sense of empowerment. When you’re feeling more confident, it’s a little easier to tune into how your body is feeling.
Breast cancer is considered stage IV, or metastatic, when it spreads beyond the breast and nearby lymph nodes to other organs in the body. 20-30% of early-stage breast cancers later become metastatic. In the U.S., 6% of first-time breast diagnoses are stage IV. This is called de novo metastatic breast cancer.
After a metastatic breast cancer diagnosis, sometimes the first thing people look for is information on how many years they may live. This is completely understandable. Still, other people prefer not to research this topic. If you do choose to read about life expectancy after a metastatic breast cancer diagnosis, it’s important to know that your unique situation could be very different than what you see in the general survival rate numbers that are currently available. If you’re concerned about life expectancy, talk with your doctor. Ask to have a candid discussion about it. You can also ask to talk with your cancer center’s oncology social worker if you want extra support.
A key part of research after diagnosis is making sure you’re comfortable with the doctor guiding your care. Your doctor and medical team will be your partners as you navigate metastatic breast cancer tests and treatment. If you don’t yet have a medical oncologist, here are some tips for finding one:
- Ask your primary care physician for a referral.
- Talk to friends and family who may be able to recommend a breast cancer medical oncologist.
- Connect with others who’ve been diagnosed and ask for recommendations. Visit LBBC’s social media communities, where you can meet others who may have suggestions:
- Visit the American Society of Clinical Oncology’s Find a Cancer Doctor page.
- If you are seeking LGBTQ-supportive cancer treatment, visit the National LGBT Cancer Network’s care directory.
Your research should include looking at the doctor’s education and years of experience and hearing feedback from people who’ve seen the doctor. But the right fit isn’t only about experience. If the doctor seems like a good fit on paper, meeting in person can also help you decide. For instance, what does it feel like to have a conversation with this person? Are your concerns being heard? Do you feel a sense of trust and support? Consider this as you do your research and meet potential physicians.
“Metastatic breast cancer is a complex disease that requires patients and physicians to work collaboratively in order to minimize side effects and maximize quality of life,” says Saveri Bhattacharya, DO. “It is important that physicians know a patient's values and a patient understands the disease trajectory.”
If you are under the care of a medical oncologist now, but you’re not sure it’s the right fit, seeking a second opinion is a good way to explore other possible doctors.
No matter what your starting point is, Living Beyond Breast Cancer is here to guide you through comprehensive information about metastatic breast cancer so you can start to make a plan and move forward.
It took me a while to digest the indefiniteness of a metastatic diagnosis. But once I understood, I accepted my reality and was able to continue to start living in the moment. That is the challenge.
- Nazneen
Recommended reading
| Emotional support | Anxiety | Financial matters |
| Exercise | Sex & intimacy | Talking with family |
Learning to adapt over time
It takes time to adjust to a metastatic breast cancer diagnosis. It’s a shift that can feel deep and layered. Trying to learn a lot of new information while processing intense emotions is not a normal experience! It’s important to pace yourself, take breaks, and to know when to reach out for support.
Part of adapting to your diagnosis is learning to recognize symptoms and treatment side effects. Some of these can mimic symptoms of other conditions, so it’s always important to let your healthcare team know what you’re experiencing.
Depending on where cancer is in your body, symptoms can include:
- Fatigue
- Appetite or weight loss
- Bone pain and fractures
- Shortness of breath
- Dry cough
- Loss of balance
Common treatment side effects include:
- Fatigue
- Nausea
- Reduced immune function
- Sexual side effects such as low libido or vaginal dryness
- Hair loss
- Difficulty focusing and remembering
- Anxiety or depression
There are many other possible symptoms and side effects, so tell your doctor or nurse about anything that feels out of the ordinary. Together, you can create a plan that can help you feel better.
Adapting to a diagnosis of metastatic breast cancer is a series of ongoing adjustments over days, months, and years. It’s not uncommon to realize one day that you’ve come through changes you never anticipated facing, and that you have new emotional muscles. You may discover that you’ve been able to walk into, and through, many periods of uncertainty — a skill some people spend a lifetime trying to master.
Metastatic breast cancer is a marathon. There are times when it’s flat ground and it’s easy, and times when you’re running uphill. We just don’t know what's around the corner anymore, because the pace of change is faster than at any time in the history of cancer treatment.
- Pallav Mehta, MD
New treatment options for MBC
Although metastatic breast cancer isn’t curable, it is treatable. The goal of treatment is to keep the cancer under control while reducing symptoms and side effects so you can have the best possible quality of life.
There are many different kinds of treatments available for metastatic breast cancer, including:
Research is changing the treatment of metastatic breast cancer. It may be surprising to learn that most people starting treatment for metastatic breast cancer do not begin with chemotherapy. Many people start with hormonal therapy or targeted therapy.
Among the newer metastatic breast cancer treatments that have been developed because of research are these targeted therapies:
- PARP inhibitors: These medicines cause cancer cells to die by preventing them from fixing damaged DNA. PARP inhibitors are approved to treat metastatic breast cancer in people who have an inherited BRCA1 or BRCA2 genetic mutation.
- PIKC3A inhibitors: These treatments are approved to treat certain metastatic breast cancers whose tumor cells have a mutation in the PIK3CA gene. PIKC3A inhibitors disrupt the activity of an enzyme called P13 kinase, interfering with cancer cells’ ability to grow.
- Trop-2 antibody-drug conjugates: This drug combination targets a protein called Trop-2, often found in triple-negative breast cancers. These treatments combine the Trop-2 antibody and a chemotherapy drug so that chemotherapy can be delivered directly to certain cancer cells.
These are just a few examples. You and your healthcare team can work together to create a tailored treatment plan for you. If the cancer’s response to treatment changes over time, your plan can be adjusted to help ensure you’re continuing to receive the most effective treatment. And any time you’re considering a treatment is a good time to ask your doctor about opportunities to participate in a clinical trial. Clinical trials provide access to treatments that may be very effective but are not yet FDA-approved.
“I think the most exciting aspect of metastatic breast cancer management for the near and mildly distant future is the further refinement of genomically driven treatment,” says Pallav Mehta, MD. “Breast cancers, like most solid tumors, often have several driver mutations and continue to acquire new mutations as the cancer progresses. We're getting better not just at identifying these mutations, but also at understanding what these aberrant genes actually do to the cell. And we’re getting better at designing drugs that can target the protein product of these genes.
“A second exciting advance is in the field of immunotherapy, which is a way to have the patient's own immune system wake up from the stupor induced by the cancer and do its job, which is to protect the house,” says Dr. Mehta. “CAR T-cell therapy [immunotherapy that alters a person’s immune cells to target cancer] is exciting, checkpoint inhibitors are showing some promise, and even vaccines have relevance again.”
Learn more about treatment options and read the latest treatment news.