Four Steps at a Glance
Refer to the following pages for detailed steps.
|
Step 1: Ask the two age-specific screening questions - One about friends' drinking - One about patient's drinking frequency |
|
\/
| NO |
<- Does the patient drink? -> | YES |
|
Step 2: Guide Patient For patients who do not drink alcohol |
Step 2: Assess Risk For patients who do drink |
|
If friends drink:
If friends don't drink:
|
|
| Screening complete for patients who do not drink | Step 3: Advise and Assist |
|
Lower Risk
Moderate Risk
Highest Risk
|
|
Step 4: At Followup, Continue Support |
|
Step 1: Ask the Two Screening Questions
Research indicates that the two age-specific screening questions (about friends' and patient's drinking) are powerful predictors of current and future alcohol problems in youth. Fit them into your office practice in whatever way works best for you, whether by adding them to a pre-visit screening tool or weaving them into your clinical interview. In either case, take steps to protect patient privacy and, if at all possible, conduct an in-person alcohol screen when you are alone with your patient. See page 25 for more information about confidentiality.
Guidelines for asking the screening questions: (1) For elementary and middle school patients, start with the friends question, a less threatening, side-door opener to the topic of drinking. (2) Because transitions to middle or high school increase risk, choose the question set that aligns with a patient's school level, as opposed to age, for patients aged 11 or 14. (3) Exclude alcohol use for religious purposes.
|
Elementary School Ask the friends question first. |
Friends: Any drinking? "Do you have any friends who drank beer, wine, or any drink containing alcohol in the past year?" ANY drinking by friends heightens concern. |
Patient: Any drinking? "How about you - have you ever had more than a few sips of beer, wine, or any drink containing alcohol?" ANY drinking: |
|
Middle School (Aged 11-14) Ask the friends question first. |
Friends: Any drinking? "Do you have any friends who drank beer, wine, or any drink containing alcohol in the past year?" ANY drinking by friends heightens concern. |
Patient: How many day? "How about you - in the past year, on how many days have you had more than a few sips of beer, wine, or any drink containing alcohol?" ANY drinking: Moderate or Highest Risk (see chart on page 10) |
|
High School (Aged 14-18) Ask the patient question first. |
Patient: How many day? "In the past year, on how many days have you had more than a few sips of beer, wine, or any drink containing alcohol?" Lower, Moderate, or Highest Risk (see chart on page 10) |
Friends: How much? "If your friends drink, how many drinks do they usually drink on an occasion?"
Binge drinking by friends heightens concern. (3 to 5+ drinks; see page 15) |
| NO |
<- Does the patient drink? -> | YES |
| Go to Step 2: Guide | Go to Step 2: Assess Risk |
Step 2: Guide Patient
For patients who DO NOT drink...
| NO |
<- Do friends drink? -> | YES |
|
Neither patient nor patient's friends drink
|
Patient does not drink, but friends do
|
|
|
|
| Screening complete for nondrinkers |
Step 2: Assess Risk
For patients who DO drink...
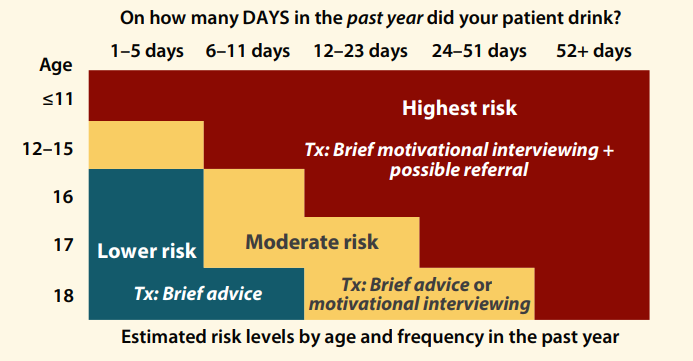
For a broad indicator of your patient's level of risk, start with the chart below, which provides empirically derived population-based estimates. Then factor in what you know about friends' drinking and other risk factors, ask more questions as needed, and apply your clinical judgment to gauge the level of risk.
In the chart, see where your patient's age and drinking frequency intersect: If your patient responds to the screening question with a per-month or per-week frequency, convert the answer to days per year to see where the drinking falls on the risk chart. As an example, a 15-year-old who reports drinking about twice a month, or 24 days in the past year, is at “highest risk” for adverse consequences. (This chart is also in the Pocket Guide; see page 19 for tips on remembering the risk level cut points.)
Factor in friends:
- For elementary and middle school students: Having friends who drink heightens concern. Because having more drinking friends means more risk, ask how many friends drink, if your patient didn’t offer this detail when answering the screening question.
- For high school students: Having friends who binge drink heightens concern. Recent research estimates that binge drinking levels for youth start at 3 to 5 drinks, depending on age and gender (see page 15).
Include what you already know about the patient’s physical and psychosocial development in your risk evaluation, along with other relevant factors such as the level of family support, drinking and smoking habits of parents and siblings, school functioning, or trouble with authority figures.
For moderate risk and Highest risk patients:
- Ask about their drinking pattern: : “How much do you usually have? What’s the most you’ve had at any one time?” If the patient reports bingeing (see page 15), ask: “How often do you drink that much?”
- Ask about problems experienced or risks taken: “Some people your age who drink have school problems like lower grades or missed classes. Some do things and feel bad about them later, like damaging or stealing property, getting into fights, getting sexually involved, or driving or riding in a car driven by someone who has been drinking. Others get injured, have memory blackouts, or pass out. What not-so-good things related to drinking, if any, have you experienced?”
- Ask about other substance use (“Have you used anything else to get high in the past year?”) and consider using other formal tools to help gauge risk (see page 32). The majority of your lower risk patients will not have used illicit drugs (NIAAA, 2011), but ask them, too, about past-year use, time permitting.
Step 3: Advise and Assist
For patients who DO drink...
| Lower Risk |
Moderate Risk |
Highest Risk |
|
|
|
For All Patients Who Drink
|
If you observe signs of acute danger, such as drinking and driving, high intake levels per occasion, or use of alcohol with other drugs, take immediate steps to ensure safety (see page 21). |
|
Step 4: At Followup, Continue Support
For patients who DO drink...
| NO |
<- Was patient able to meet -> and sustain goal(s)? | YES |
|
Patient was not able to meet and sustain goal(s):
|
|